There are now two medications licenced for weight loss in the UK that really work.
Until now, we simply haven’t had anything useful and the new medications are really changing the landscape for the management of overweight and obesity.
Both of these medications, Semaglutide (Wegovy) and Tirzepatide (Mounjaro) have been available for treating type 2 diabetes for a few years, but in higher doses they are now used for weight loss and weight loss maintenance.
These medications work on the hormones that control our hunger and our satiety (fullness).
Our gut, brains and other body organs work together to give us hunger signals and satiety signals. The science of this is rapidly advancing and it is this knowledge that has allowed development of new medications.
There are two areas in our brain that do a lot of the “processing”
Agouti-related protein (AgRP) and Neuropeptide y (NPY)
Causes increased hunger and food-seeking behaviour and down – regulates energy expenditure
Pro-opiomelanocortin receptors (POMC) and cocaine and amphetamine-regulated transcript (CART)
Downregulates hunger and causes satiety and increased energy expenditure
These areas are under the influence of a large number of chemical messengers and hormones, and it is some of these that are targeted in the new medications and will have differing effects on our bodies.
So far, the medicines target two different areas
Semaglutide works by making the body think it has more GLP-1 – which is glycagon-like peptide -1, a hormone that makes us more full and less hungry.
Tirzepatide targets both GLP-1 and GIP which is glucose-dependent insulinotropic polypeptide. Again, this has the action of making us less hungry and more full.
These medications make our bodies
Produce more insulin , the hormone that helps us to manage sugar in our diet, this is why they can be used to manage type 2 diabetes
Slow down the emptying of our stomach. This makes us feel full for longer (increases our satiety)
Reduces level of inflammation in the body.
There are a number of studies coming out all of the time showing that these medications may also have a role in reducing cardiovascular disease, improving symptoms in one type of heart failure and improve some types of liver disease associated with overweight and obesity (MASLD, Metabolic dysfunction-associated steatotic liver disease).
If you want to read the science, this is a link to the study regarding cardiovascular disease , here is a link to the heart failure trial and here is one for liver disease
Yes, they really work, which is why they are really changing the management of overweight and obesity.
Semaglutide
The average weight loss 14.9% of bodyweight.
This trial , published in the New England Journal of Medicine in 2021, was the first big trial to demonstrate that it worked.
Tirzepatide
The average weight loss is 20.9% of bodyweight.
This trial, published in the New England Journal Of Medicine 2022, was the first to prove the effectiveness of Tirzepatide.
In studies so far, Tirzepatide has been shown to be more effective for weight loss than semaglutide
These amounts of weight loss are hugely significant, both in terms of improved health and how we feel.
Improved joint pain (due to weight loss but also reduced inflammation in our bodies)
For those struggling with their pelvic floor control, weight loss will improve issues with incontinence and leaking
Reduced risks of cancer that are more common in those with overweight and obesity, such as breast cancer, Endometrial cancer (the lining of the uterus), bowel cancer, kidney cancer and pancreatic cancer.
Improved blood pressure and cholesterol levels
Reduced acid reflux symptoms
These medications are injected once a week, starting at a low dose and increasing the dose every 4 weeks until the maximum dose is reached.
For Wegovy the dosing schedule is 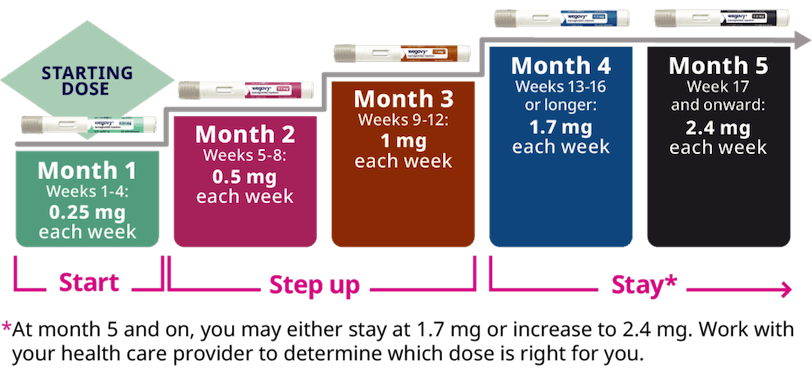
https://www.wegovy.com/taking-wegovy/dosing-schedule.html
For Tirzepatide the dosing schedule is
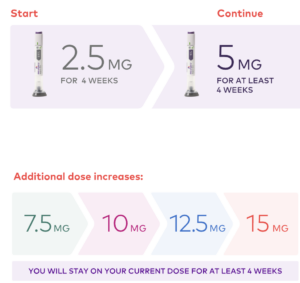
https://mounjaro.lilly.com/how-to-use-mounjaro
Both medications are prescribed in a “pen” that you use according to the instructions and inject it under the skin. It doesn’t really hurt at all.
There are some people prescribing “compounded” versions, that are in a a vial that you have to draw up into a needle. These are more risky and although cheaper, we wouldn’t recommend that you use these.
There are also some counterfeit medicines in circulation, ensure that you get from a reputable provider privately (we will cover how to check that later)
Weight loss can happen at lower doses than the maximum dose, and it may be that balancing side effects vs weight loss is a discussion you need to have with your provider, as the side effects may worsen as the dose increases
The good stuff!
We know that obesity causes hunger, because the hormones that make us feel more hungry and less full are changed by having increased fat tissue on our body.
For some people this may be the first time in a very long time that they haven’t felt hungry most of the time, which can feel very liberating. You may be less tempted to snack and your meals will almost certainly be smaller. It is important to eat, however, and to make sure you drink plenty of non-caffeinated fluids to stay hydrated.
The less good stuff
The most common side effects of these medications involve the gastro-intestinal tract. The slower stomach emptying, making you feel more full, can sometimes be uncomfortable and for a few people this can cause vomiting and abdominal discomfort. Diarrhoea can be an issue for some people.
Nausea can also be problematic.
Some people feel that their heart may beat a bit faster. This is unlikely to be dangerous but if it goes very fast, its important to seek medical help.
A few people report feeling very fatigued.
Semaglutide has been used for type 2 diabetes for over 10 years and there haven’t been many very serious side effects reported. Tirzepatide has been used for less time.
There are a few side effects that need to be looked out for because they can be serious, although they are rare.
Tirzepatide can cause hypoglycemia (low blood sugar), pancreatitis, kidney failure, allergic reactions, and vision changes. Semaglutide can cause pancreatitis, kidney failure, hypoglycemia, gallbladder issues, allergic reactions, and vision changes
If you develop severe abdominal pain or feel unwell whilst taking the medication, it is really important to discuss this with a medical professional.
People with previous thyroid cancer are not allowed to use these medications at the moment due to a theoretical risk of medullary thyroid cancer. Because the numbers of this type of cancer are so low, it has been difficult to work out whether this is a real risk, but a cautious has been taken.
At the moment it is almost impossible to get Semaglutide or Tirzepatide on the NHS for weight loss (they are used for treatment of type 2 diabetes in lower doses)
In theory, semaglutide is available through Tier 3 weight loss services for 2 years if you have health problems due to your weight and you have a BMI of either:
35 or more, or 32.5 or more if you’re of Asian, Chinese, Middle Eastern, Black African or African-Caribbean origin
30 to 34.9, or 27.5 to 32.4 if you’re of Asian, Chinese, Middle Eastern, Black African or African-Caribbean origin, and you meet other criteria to be treated by a specialist weight management service
Unfortunately, there are very few Tier 3 services prescribing Semaglutide (some are prescribing Liraglutide, an older, less effective GLP-1 medication) and 50% of the population is not able to access a Tier 3 weight loss service.
Your GP cannot prescribe these medications at present, for weight loss. This however may change and we will update this as soon as anything changes.
There are a multitude of organisations that are privately prescribing semaglutide and tirzepatide at the moment.
Some of these providers use prescribing pharmacists and some use doctors. Do not use any provider that doesn’t do this.
In general, the cost per month of the medication will increase as the dose increases and there isn’t a huge amount of variation between providers. Some are doing “bundle” offers, but the usual rule of “its too good to be true” stands here – if somewhere is selling the medication very cheaply, it is unlikely to be a genuine product.
The things to look out for when choosing a provider are:
Do they name their prescribing pharmacist or Dr? You should be able to see this information on their website.
They should ask you about your medical history to ensure it is safe for you to have this medication.
Do they offer advice around weight loss, for example what foods to focus on or any other information regarding exercise? This is the sign of a good provider who wants to maximise your health.
How do they know you have obesity or overweight? Some providers will ask you to submit photographs, some will ask for your weight and height. Some will want GP information to check. None of this is wrong, but the usual caveats about providing health data and photographs to a company on the internet apply – look for reviews online and don’t send anything if you are not sure. The only way to actually verify that you have overweight or obesity is for them to offer a video or in person consultation with you. This is the best way to ensure safe prescribing, but not all companies will do this and will have come up with their own processes. If they are not asking any questions , that should ring alarm bells.
Do they offer online or phone help? These are prescription only medications and there needs to be a way for you to contact someone if you are having issues
Do they ask to share information with your GP? Whilst some people find this difficult because they may have encountered medical obesity stigma, or don’t want their GP to know they are taking the medication, it is good practice for the company to ask, and if you feel able, it is best if you do allow the company to share info with your GP so that they know you are using it if they need to see you for other health conditions. If you choose not to share, please make sure you tell any medical professional you see that you are taking the medication to ensure that they can help you safely. You may find that this is a difficult thing to do, and that is understandable, but it is for your benefit so that no mistakes are made in diagnosing or treating any problems you have due to them not knowing what medications you are taking.
Most importantly, if you have any severe side effects, please seek medical help asap and let them know you are taking the medications.
When you take these medications, your appetite will reduce significantly, and this will increase as the dose becomes higher.
This can be lifechanging if you have always been ruled by your appetite, however it is really important that you get enough nutrition in your body, even with a lower food intake.
Some good rules to follow to maintain optimum health are:
Ensure you stay hydrated. You will be getting less water in your food, so making sure you drink enough fluids during the day is really important. Ideally about 3L of non-caffeinated fluid.
When you choose your meals, ideally eat good quality protein first, then vegetables and then the carbohydrate part of a meal. This is to ensure you are getting enough protein and vitamins and minerals. There is no one way of eating better than any other for weight loss according to all research, what is important is that you get enough energy to live your life and nutrients.
If you are struggling to get enough food into your body daily, it would be a good idea to take a multivitamin. If you are having periods, then a iron supplement as well. There is no official guidance on this, but some people find that they eat so little that there is a risk of nutritional deficiency and this will ensure that your get the micronutrients you need.
Make sure you stay as active as your body allows. As you lose weight, you may find this becomes easier. It is very important when you are losing weight, that you don’t lose muscle mass, as this can store up problems for the future. It is therefore a good idea to ensure you do some resistance or weight bearing exercise. Include some guides to good exercise for different body types. Doing activity until you become breathless is also important to help your heart and lungs remain healthy. Make sure you stay well hydrated when you are active.
If you are taking these medications after some weight regain post-metabolic bariatric surgery, it is even more important to take your vitamin supplements as you were instructed after the original surgery.
If you are struggling with the reduced volumes of food or the psychological impact of weight loss, please seek help. If you have had obesity for a long time, these things can bring up strong emotions and it is really important not to face this alone. It can also cause tension in established relationships if one person loses a lot of weight. The provider of your medication may be able to offer some talking therapies but please see your GP if you are struggling or if you are getting any suicidal thoughts or self harm thoughts, please seek emergency help via ED or the Samaritans. (put in links)
Some people find alcohol has a different or more potent effect on these medications, so be very aware of this if you choose to drink alcohol.
The trial data does show that, like after all forms of weight loss, weight regain can occur. As trials continue, we will find out more information on the real-life experiences of people, but it is important to know that this isn’t “failing”.
When weight is regained after a diet, people often self-criticise, even though the science tells us that your body will do everything it can to regain weight. It will alter the gut=-brain hormones we talked about earlier, to make you more hungry and less full. This is to try to get you to regain the weight, and a bit more. This pattern is so familiar to those who have been on many “diets” over the years. It is physiology, not willpower that is the issue.
After stopping weight loss medications, you will feel more hungry and less full again – not because you have suddenly changed who you are, but because the medication was changing your appetite. It is the same as blood pressure going up again if you stop medication for that. It really is that simple.
So, what can we do to help weight regain?
The resistance and cardiovascular activity mentioned above is really important. Exercise is not good for weight loss, but it is really helpful for managing weight regain So exercising or staying active as much as possible, and ensuring that you keep your muscles strong (even if that means chair bound activity) is important. Whatever activities you can find time for and enjoy, are the ones you are most likely to continue.
You will have eaten differently when on the medication and perhaps found new tastes for foods and learned to try the protein first method. This is good to continue when you stop the medications because protein and good fats release hormones to help you feel full for longer.
We don’t have long term safety data on these medications yet, but the 2 year rule that was introduced for semaglutide was not because it was dangerous after 2 years, but because the trials were 2 years long.
Whenever we take a medication, we need to balance the benefits vs the risks. We know there are significant benefits to using these medications and over time, we will learn more about the risks. As long as you are getting good nutrition and not becoming unwell due to losing too much weight, you do not have to stop.
Some people are finding that they use the medication in bursts to maintain weight loss. They may start again for a few weeks or months if they regain weight, and then stop again. Or, they choose to stay on a low dose. We have no data on safety or efffectiveness regarding this type of use at the moment, but hopefully it will come with time.
As we learn more about the health benefits of these medications, it may be that they are prescribed for more and more conditions such as heart disease, kidney disease and liver disease, alongside obesity. We need more research on this and it is a rapidly moving field.
We use cookies on our website to give you the most relevant experience by remembering your preferences and repeat visits. By clicking “Accept All”, you consent to the use of ALL the cookies.
Accept All